Why They Happen and How to Heal Naturally
Executive Summary
Gallbladder problems are often misunderstood as sudden events that require medication or surgery. In reality, gallbladder dysfunction usually develops slowly, driven by years of dietary choices, metabolic imbalance, digestive stress, and altered bile flow. The gallbladder itself is not the problem—it is a messenger, reflecting how well the body digests fat, regulates insulin, manages inflammation, and maintains coordinated organ function.
This paper explains, in simple language, how the gallbladder works, why common modern eating patterns—especially prolonged low-fat, high-carbohydrate diets—can quietly impair bile flow, and how early gallbladder dysfunction can often be stabilised or reversed when addressed systematically. Rather than focusing on isolated symptoms, a functional health and longevity perspective looks at how liver function, metabolic regulation, gut health, nervous system tone, hormonal balance, inflammation, detoxification capacity, and circadian rhythm interact to determine gallbladder health.
When bile flows well, fat digestion improves, fat-soluble vitamins are absorbed, inflammation settles, and metabolic balance returns. When bile stagnates, digestion becomes strained, cholesterol concentrates, stones can form, and pain or inflammation may follow. The encouraging reality is that many gallbladder problems—particularly in their early stages—respond well to supportive dietary, lifestyle, and environmental changes when these are introduced thoughtfully and progressively.
This paper provides a clear, practical, and hopeful framework for understanding gallbladder dysfunction and restoring digestive resilience, metabolic flexibility, and long-term health.
Understanding the Gallbladder’s Role in Human Physiology
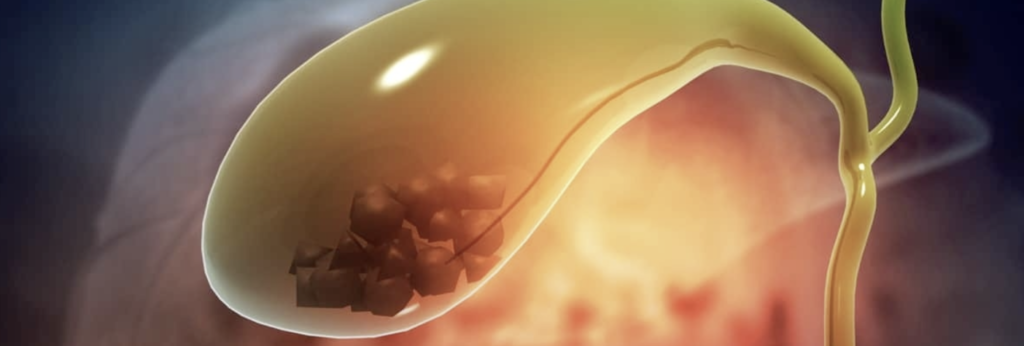
The gallbladder is a small, pear-shaped organ located just beneath the liver. Its primary role is to store and concentrate bile, a yellow-green fluid made by the liver. Bile is essential for digestion because it allows dietary fats to be broken into tiny droplets that digestive enzymes can act on. Without adequate bile flow, fats pass through the digestive tract poorly digested, leading to bloating, discomfort, nutrient deficiencies, and metabolic stress.
When a meal containing fat is eaten, the gallbladder contracts and releases bile into the small intestine. This coordinated response allows fats to be absorbed efficiently and enables the uptake of vitamins A, D, E, and K—nutrients critical for immune function, hormone balance, bone health, brain function, and cardiovascular protection.
From a systems perspective, the gallbladder does not operate independently. Its function depends on liver health, insulin signalling, nervous system input, gut integrity, hydration status, and daily eating patterns. When these systems fall out of balance, bile flow can slow, thicken, or stagnate, setting the stage for dysfunction.
How Gallbladder Dysfunction Develops Over Time
Gallbladder problems rarely appear overnight. They develop gradually as bile becomes thicker and less mobile. One of the most overlooked contributors is prolonged avoidance of dietary fat. When fat intake remains very low for extended periods, the gallbladder receives little stimulus to contract. Bile remains stored for too long, becomes concentrated, and may form sludge—thickened bile that is the precursor to stone formation.
At the same time, modern diets high in refined carbohydrates and sugars raise insulin levels. Elevated insulin signals the liver to produce more cholesterol, some of which enters bile. When bile becomes overly saturated with cholesterol and remains stagnant, cholesterol crystals can form, eventually developing into gallstones.
This process is strongly influenced by metabolic health. Insulin resistance, blood sugar instability, and chronic inflammation alter bile composition and impair gallbladder motility. Over time, this can lead to biliary sludge, gallstones, inflammation of the gallbladder wall, or impaired contraction, even in the absence of visible stones.
From a functional standpoint, gallbladder dysfunction reflects a mismatch between how the body is designed to process fats and how modern eating patterns often restrict or distort fat intake.
Common Signs and Symptoms of Gallbladder Stress
Gallbladder dysfunction often presents subtly at first and is frequently mistaken for acid reflux or general indigestion. Symptoms may include bloating after meals, particularly meals containing fat, discomfort or sharp pain in the right upper abdomen or right shoulder, nausea, burping, or a sense of heaviness after eating. Some individuals notice pale or greasy stools, an early sign that fat digestion is impaired. Others feel full very quickly or develop an increasing intolerance to fatty foods.
In more advanced cases, inflammation or infection can cause fever, chills, or more severe pain. These symptoms are signals, not failures. They indicate that bile flow and digestive coordination need support.
A functional health approach recognises these signs early and uses them as clues to underlying system imbalance rather than waiting for structural damage to occur.
The Most Common Gallbladder Conditions Explained Simply
Gallstones form when bile components crystallise, usually due to cholesterol saturation and poor bile movement. Some stones remain silent, while others obstruct bile flow and cause acute pain. Biliary sludge represents thickened bile that has not yet hardened into stones but still interferes with gallbladder function. Cholecystitis refers to inflammation of the gallbladder, often triggered by blocked bile ducts, and may require urgent care if infection develops. Biliary dyskinesia describes poor gallbladder contraction, where bile is present but not released efficiently.
Importantly, these conditions often exist along a spectrum rather than as isolated diagnoses. Addressing them effectively requires understanding where along this continuum an individual sits and what upstream factors are driving dysfunction.
Can Gallbladder Function Be Restored Naturally?
In many cases, especially before severe inflammation or large stone formation, gallbladder function can improve significantly when the body is supported correctly. Restoration is not about forcing bile flow aggressively but about re-establishing healthy signalling between the liver, gallbladder, gut, and metabolic system.
Gradually reintroducing healthy dietary fats is central. Fats such as olive oil, avocado, egg yolks, fatty fish, and coconut oil gently stimulate gallbladder contraction, keeping bile mobile. Introducing these slowly allows the gallbladder to regain rhythmic function without triggering discomfort.
Bitter foods play a valuable role by naturally stimulating bile production and flow. Leafy greens such as arugula, dandelion, and radicchio, along with traditional bitter herbs like artichoke leaf and gentian, support liver-gallbladder coordination and digestive readiness.
Maintaining stable blood sugar and insulin levels is equally important. Diets that reduce refined carbohydrates and excess sugars lower cholesterol saturation in bile and reduce stone-forming risk. Hydration supports bile fluidity, preventing thickening and stagnation.
Intermittent fasting, when practised thoughtfully and followed by adequate fat intake, can allow digestive organs to rest and reset. Gentle daily movement supports abdominal organ circulation and lymphatic flow, indirectly assisting bile movement.
In cases of significant digestive sluggishness, temporary use of bile salts or ox bile under professional supervision may assist digestion while underlying function is restored.
A functional health and longevity coach integrates these strategies carefully, tailoring pace and sequence to the individual’s digestive tolerance, metabolic state, stress load, and medical history.
When Medical Intervention Becomes Necessary
Despite best efforts, some cases progress to the point where imaging, medication, or surgery is required. Ultrasound can identify stones, blockages, or infection. In selected cases, bile acid medications may help dissolve cholesterol stones over time. When the gallbladder becomes severely inflamed, infected, or nonfunctional, surgical removal may be necessary.
Living without a gallbladder is possible, but bile then flows continuously rather than being released in a controlled manner. Long-term digestive support is often needed to maintain fat absorption, gut health, and metabolic balance. Functional guidance remains valuable even after surgery, helping the body adapt and thrive.
Gallbladder Health as a Marker of Longevity
The gallbladder’s role extends beyond digestion. Efficient bile flow supports metabolic flexibility, cholesterol balance, inflammation regulation, gut health, hormone signalling, and detoxification. From a longevity perspective, gallbladder health reflects how well the body processes fuel, manages stress, and adapts to dietary inputs over time.
Rather than viewing gallbladder issues as isolated mechanical failures, a functional systems approach recognises them as opportunities to restore alignment across the body’s interconnected networks. When diet, lifestyle, environment, and daily rhythms support physiology rather than fight it, the gallbladder often recovers its natural role quietly and effectively.
Gallbladder problems do not need to define the future. With understanding, patience, and the right support, many people reclaim comfortable digestion, improved energy, and renewed metabolic resilience—benefits that extend far beyond the gallbladder itself.
References
Carey, M.C. & Small, D.M. (1978). The physical chemistry of cholesterol solubility in bile. Journal of Clinical Investigation, 61(4), pp.998–1026.
Hofmann, A.F. (1999). The continuing importance of bile acids in liver and intestinal disease. Archives of Internal Medicine, 159(22), pp.2647–2658.
Portincasa, P., Moschetta, A. & Palasciano, G. (2006). Cholesterol gallstone disease. The Lancet, 368(9531), pp.230–239.
Shaffer, E.A. (2005). Epidemiology and risk factors for gallstone disease. Best Practice & Research Clinical Gastroenterology, 20(6), pp.981–996.
Di Ciaula, A., Wang, D.Q. & Portincasa, P. (2018). An update on the pathogenesis of cholesterol gallstone disease. Current Opinion in Gastroenterology, 34(2), pp.71–80.
Cordain, L. et al. (2005). Origins and evolution of the Western diet. American Journal of Clinical Nutrition, 81(2), pp.341–354.
Jones, P.J.H. & Rideout, T.C. (2014). Lipids, sterols, and bile acids. In: Modern Nutrition in Health and Disease. Philadelphia: Wolters Kluwer.
About Mathew Gomes
Functional Health, Nutrition & Longevity Coach
Mathew Gomes is a Functional Health, Nutrition & Longevity Coach helping busy professionals reverse early health decline before it becomes disease. Trained in Functional Nutrition Coaching (AAFH) and certified in executive coaching (ICF, EMCC), with an engineering background and MBA, he brings systems thinking and strategic clarity to health restoration.
Shaped by senior leadership experience and a personal health crisis, Mathew uses functional assessment and targeted testing to identify root causes and coordinate personalised nutrition, metabolic repair, strength training, nervous-system regulation, sleep and recovery. He works alongside doctors for diagnosis and medication while building resilient, sustainable health—so clients regain energy, focus and confidence without guesswork.
Disclaimer
This white paper is provided for educational and informational purposes only. It is not intended to diagnose, treat, cure, prevent, or provide medical advice for any disease or health condition.
The author is a Functional Health, Nutrition and Longevity Coach, not a medical doctor. The content presented reflects a functional, educational perspective on health, lifestyle, nutrition, and risk factors, and is designed to support informed self-care and productive conversations with qualified healthcare professionals. Nothing in this document should be interpreted as a substitute for medical advice, diagnosis, or treatment from a licensed physician or other qualified healthcare provider. Readers should not start, stop, or change any medication, supplement, or medical treatment without consulting their prescribing clinician.
Individual responses to nutrition, lifestyle, supplements, and coaching strategies vary. Any actions taken based on this information are done at the reader’s own discretion and responsibility. If you have a medical condition, are taking prescription medication, or have concerns about your health, you are advised to seek guidance from a licensed healthcare professional before making changes.